Know Your Skin

Your skin is your first line of defense against infection. The many layers of skin provide different types of protection. The first layer, known as the epidermis, is your immune system’s shield, protecting your body from the onslaught of infectious bacteria, viruses, yeasts, parasites, and fungi that are nearby. The second layer of skin, the dermis, supports your skin’s surface, supplying it with nutrients and making it tougher. The third and final layer of skin is the subcutaneous zone. This is a layer of fat that acts like a shock absorber, keeps your temperature steady, and stores energy. All of your skin layers work together to ward off skin infections.
How Does Your Skin Get Infected?

A tiny cut is all it takes to provide an invading microorganism entry into your skin. Often this is how a skin infection takes root. Sometime the cut is not so tiny, like after you’ve had surgery. In any case, your skin is more vulnerable to infections when it has been broken in some way.
Infections usually come from one of three main causes: bacteria, viruses, and fungi. Yeasts and parasites can cause them, too. Many of these are harmless on the surface of your skin, and bacteria in particular are plentiful on all human skin. But when they enter a break in the skin, trouble can start. Sometimes a break in the skin isn’t necessary, and sometimes a microorganism invader gains an upper hand because your immune system is weak, or is misdirected into attacking the wrong things. Causes of skin infections can be complex.
How Are Skin Infections Treated?

For bacterial skin infections, your doctor may prescribe antibiotics. However, antibacterial-resistant bacteria have become a growing problem, especially in hospitals. Fungal skin infections can be treated with antifungal medicines, also known as antimycotic agents. These include pills and creams, some of which are prescribed and some of which can be purchased at a drug store without a prescription. For viral infections, your doctor may use antiviral medicine, or may remove the growth itself. Sometimes a skin infection goes away naturally without medical intervention.
MRSA
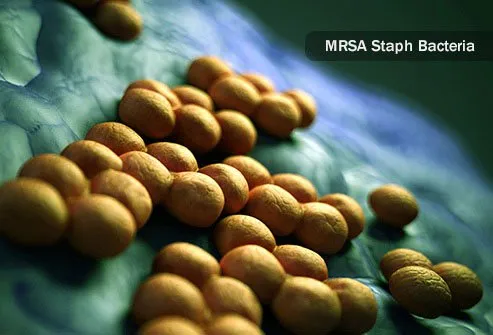
MRSA (methicillin resistant Staphylococcus aureus) is a type of staph infection that resists typical antibiotics. These bacteria have developed a gene called mecA that keeps standard antibiotics like penicillin and others from binding to the bacteria. MRSA is no more harmful than any other staph infection, except that it cannot be easily treated. Most MRSA bacterial infections happen in hospitals and nursing homes, where ill and elderly patients are especially vulnerable to infection. These infections can sometimes be acquired at tattoo parlors, schools, and military barracks as well.
Cellulitis (Erysipelas)

Caused by a bacterial infection, cellulitis triggers skin redness, swelling, and tenderness. It makes your skin feel hot, and the infection spreads rapidly. Some describe the skin as having the dimples of an orange peel. Some people have confusion, fever, and an abnormally fast heartbeat hours before the skin symptoms develop. It usually occurs on the arms or legs. This can be a serious skin condition and can lead to blood poisoning, gangrene, and other life-threatening conditions like organ infection. Doctors treat cellulitis using antibiotics.
Impetigo

Impetigo is a bacterial infection that sometimes invades the body through a break in the skin, but sometimes it can set in without any skin break. It causes crusty sores mainly on the face and hands, but can appear elsewhere. Children, especially boys, are most prone to impetigo. But sometimes adults can get it too. It's most common during the summer. Outbreaks are possible, as infections can spread to many people. When there are many impetigo sores or in the case of an outbreak, oral antibiotics are called for. In milder cases, topical antibiotics may be used as treatment.
Flesh-Eating Bacteria (Necrotizing Fasciitis)

Necrotizing fasciitis, commonly called "flesh-eating bacteria," can be caused by several different types of bacteria. This is a serious skin condition, as the included photo demonstrates clearly. It results from infections deep enough to penetrate the elastic superficial fascia, your deepest layer of skin. It usually starts from a small lesion, such as a bug bite or boil, usually in legs or feet. It then typically develops into cellulitis. Eventually such an infection toxifies the body, causing high fevers, exhaustion, and disorientation. Major tissue damage follows, and death from flesh-eating bacteria is a common result, particularly if surgery is not performed quickly.
Folliculitis

Hair follicles are the skin pouches that hold your hair roots in place. When they get inflamed, the condition is called folliculitis. Bacterium, fungus, virus, yeast, and parasite infections can cause it, although it can also be caused by curly hair that's been recently shaved. Sometimes poorly maintained hot tubs can spread bacterial infections in a condition known as hot tub folliculitis. The treatment varies depending on the cause. It often goes away by itself. But for chronic folliculitis, common on the buttocks of both men and women, laser hair removal may be the best treatment option.
Boils and Carbuncles

Like folliculitis, a boil develops from an irritated hair follicle. But in the case of a boil (also called a "furuncle") the infection is much deeper, extending to the subcutaneous tissue of the skin's third layer. When several boils coalesce, we call the mass a carbuncle. Carbuncles are most common on the back of the neck, and people with diabetes are most likely to get them. Boils tend to rupture and drain on their own, but they can be coaxed with the application of moist heat, such as with a warm wash cloth. If that fails, doctors have several options for treatment, including cutting and draining the boil, and oral antibiotics. If you have boils, it is smart to regularly keep your hands clean, as these infections can spread if you aren’t careful.
Genital Herpes

The virus that causes genital herpes, HSV-2, is usually found in the anal/genital area, but not always. This is a virus infection that lasts a lifetime in your body. It usually develops after sex with an infected partner. Outbreaks cause an itching or burning feeling followed by the development of small, reddish blisters for about a week to a week and a half, during which time the virus is particularly infectious. The first outbreak is usually the worst. Between outbreaks, herpes remains in your body in a resting state. There are antiviral medicines for severe outbreaks, including Aciclovir, Valaciclovir, and Famciclovir. Avoid sex during an outbreak. If you do have sex, let your partner know ahead of time and be sure to use a condom to reduce your odds of spreading the disease.
Cold Sores

Type 1 herpes virus is more likely to develop on the face, particularly around your lips. It is extremely common, particularly in crowded parts of the world where most children have it by age 5. The initial infection is often worst, and can cause fever and restlessness. It also makes lymph glands large and tender. Like HSV-2, oral herpes is a lifelong infection that goes dormant between outbreaks. New outbreaks can be caused by stress, hormonal fluctuations, and sickness—why they are sometimes known as "fever blisters." Outbreaks go away with time, and while painful and potentially embarrassing they usually do not cause further problems. However, the virus can be spread to other areas on your body during an outbreak, so keep your hands clean to prevent this from happening. If you find the nuisance of cold sores unbearable, ask your doctor for a prescription to help control outbreaks.
Chicken Pox

The itchy chicken pox rash begins as red bumps and spots that form into blisters full of clear fluid. The clear fluid becomes cloudy over time, and eventually dries up. This leaves scabs to form and then fall away. It usually begins on your torso and face before spreading to arms, legs, and scalp. This is true of children specifically; adults may not get a rash, or it may develop in a different way. At its peak, each year this viral infection sent more than 10,000 children to the hospital before a vaccine was introduced in 1995. With 91% of very young children now vaccinated, the rate of hospitalization had declined by 93% as of 2012, according to CDC data.
Water Warts (Molluscum Contagiosum)

This viral disease, more common in childhood, causes long-lasting but relatively harmless clusters of pearl-like papules to grow on skin. The papules are known as mollusca. People who live in hot, crowded areas are more susceptible to infection, and it thrives in wet conditions. Dermatologists have a wide variety of options for treatment, though no treatment is perfect, and the virus cannot yet be killed. Treatments for molluscum contagiosum include:
- Surgical removal
- Cryotherapy (freezing)
- Laser removal
- Chemical removal
Ringworm

Ringworm is a well-known fungal infection that is common, especially in school-age children. The namesake ring-shaped rash it causes can be treated using various topical creams, as well as oral antifungal medicines in severe cases. Many ringworm medicines are available in the US without a prescription. If non-prescription methods don’t work, tell your doctor.
Athlete’s Foot

Just like ringworm, athlete's foot is caused by a fungus. In fact, several fungi can cause this itchy, burning infection. It usually grows between your toes, but can spread to your heel, and to the edges and soles of your feet as well. Athlete's foot is very common, affecting anywhere from 15% to 25% of all people at any given time. This infection can spread to other parts of the body and to other people, and many people are infected without knowing it. It’s a good idea to check your feet—particularly between your toes—for signs of cracked skin. There are several antifungal medicines used to treat athlete’s foot, and topical allylamines like terbinafine seem to be more consistently effective than other types.
Skin Parasites

Is a parasite to blame for your skin infection? Skin parasites including tiny, burrowing creatures like scabies and hookworms, and others that breed on your skin, like head lice. Itchy, red, irritated skin is a common reaction to a skin parasite. If you suspect you may have skin parasites, talk to your doctor or dermatologist about lotions, shampoos, or other medicated products for relief.
Candida (Fungal Yeast Infection)

Your body hosts Candida yeast naturally in your gut, beginning soon after you are first born. Many people have it on their skin, too, and it often lives in the mouth, throat, and vagina. It usually causes no trouble. But sometimes this yeast can set in as a skin infection, particularly in skin folds such as armpits. These infections are sometimes difficult to treat, as more and more Candida infections are resistant to common antifungal medicines.
Staph Infection (Golden Staph)

Staph infections are common. Also called "golden staph," anywhere from 15% to 40% of people have Staphylococcus aureus bacteria on their skin at any given time. But your immune system usually keeps it in check. If you have dry skin, you may be more vulnerable, as dry skin breaks easily. These breaks in skin give convenient entry to staph bacteria. Infections can be a sign of poorly controlled diabetes or other immunity problems, so if you get them frequently or severely, let your doctor know. Staph sometimes invades an open wound, causing wound infection. And nursing mothers should be particularly careful about infections on breasts, as these staph infections can be passed to children through breast milk. Staph is infectious, and if it gets into your bloodstream it can cause deadly blood poisoning (sepsis). Keep your wounds clean and covered, wash your hands frequently, and avoid sharing personal items like towels and razors.
Fifth Disease (Human Parvovirus)

You may have heard of parvovirus infections in pets, but humans cannot catch it from pets. However, parvovirus B19 is a type that does spread between humans. Children are most likely to contract fifth disease, a viral infection caused by parvovirus B19. It can cause a red rash on the face which lends it the nickname "slapped cheek syndrome." Although the disease is typically mild, it can cause serious problems for people with weak immune systems, sickle-cell disease, and other types of chronic anemia. Adults who contract it may also develop arthritis.
Leprosy (Hansen’s Disease)

Leprosy is a very slow-growing bacterial skin infection. In some cases, it takes two decades before leprosy infection causes symptoms. The body tissues most likely to be affected are the skin, eyes, nerves, and the lining of the nose. Since ancient times, leprosy has infected people. Before recently, people who developed leprosy (also called Hansen’s disease) were ostracized from friends and family for fear their bacterial infection might spread. But in the late 20th century a cure known as multidrug therapy emerged, which kills the leprosy microorganism Mycobacterium leprae. The treatment also stops the spread of the disease, allowing people with leprosy to work and live among healthy others.
Skin Infections: Types, Causes, and Symptoms
This tool does not provide medical advice. See additional information: 
© 1996-2024 WebMD, LLC. All rights reserved.
