What Is Staphylococcus?

Staphylococcus (staph) is a type of bacteria that can cause many types of infections on and in your body. Staph (pronounced "staff") is extremely common. Of every 10 people, three have it on their skin.
While it is the leading cause of skin infection, it often causes no disease. But when disease develops, if left untreated the dangers can be extremely serious.
More than 30 subspecies of Staphylococcus bacteria cause infections. The most common type of Staph infection is caused by Staphylococcus aureus. If S. aureus bacteria infect your body, either through a wound on your skin or through your airways, they can cause serious infections.
Warning: this slideshow contains some graphic images.
Who Is at Risk for Staph Infections?

While anyone can get infected with Staphylococcus, some people face a higher risk. Those populations most at risk of Staphylococcus infections include newborns, breastfeeding women, and people who:
- Have weakened immune systems
- Have certain diseases, including diabetes, vascular or lung diseases, or cancer
- Inject drugs or medications
- Have skin injuries or disorders
- Are recovering from surgery
- Use intravenous catheters
What Are the Signs and Symptoms of a Staph Infection?

To avoid these infections, you will need to know what to look for.
Skin Infections
Symptoms of staphylococcal disease of the skin include pus-filled abscesses. These are often called boils, or furuncles. Pain, swelling, and redness often target the infected area, and pus may drain from it too.
Blood Infections
Staph infection in the blood is called bacteremia or sepsis. Symptoms can include fever, chills, and low blood pressure (hypotension).
Diseases Caused by Staph

Staphylococcus can cause many different types of infections in and on around your body. Most of these infections cause localized inflammation or abscesses, which are pockets of infection.
Skin
Staphylococcus infections usually appear on your skin's surface. The most common are impetigo, a crusting of the skin, and cellulitis, which may leave your skin red and swollen.
Breast
Breastfeeding women can get a staph infection of the breast called mastitis, which can release bacteria into a mother's milk.
Lungs
Staph bacteria in the lungs can cause pneumonia.
Blood Poisoning
Staph infection in your blood can be particularly dangerous. This is commonly called blood poisoning (septicemia). These infections can spread. Internal places like your bones and organs are vulnerable to them.
Bone
When a staph infection gets into the bone it can cause osteomyelitis, a rare but serious joint infection.
Heart
Staphylococcal blood poisoning can also infect your heart or heart valves. This is called endocarditis.
Sepsis
If a staph infection gets into the bloodstream, it can spread to other organs and cause severe and life-threatening infections called sepsis or bacteremia. Sepsis can lead to shock or multi-organ failure, which can rapidly lead to death.
What Is Antibiotic-Resistant Staphylococcus aureus?

Methicillin-resistant Staphylococcus aureus, often abbreviated to MRSA, is a type of staph bacteria. MRSA is considered a type of "superbug," because it has become resistant to antibiotics commonly used to treat it. Those antibiotics include methicillin, from which it gets its name, and also penicillin, amoxicillin, and oxacillin and possibly others.
MRSA causes illness in hospitals, nursing homes, prisons and other health facilities. These are called HA-MRSA (healthcare-associated methicillin-resistant Staphylococcus). It has also caused infections outside of healthcare facilities. These cases are called CA-MRSA (community-associated methicillin-resistant Staphylococcus.
Scalded Skin Syndrome

Skin infections with staph bacteria can cause a serious condition called scalded skin syndrome. This is seen more often in children, but can occur in adults as well. The infection causes a breakdown of the upper layers of the skin, which blisters and sloughs off, just like a severe burn.
When the infection covers a large surface area of the body, the result can be fatal. Scalded skin syndrome is treated with intravenous antibiotics and fluids to prevent dehydration.
What Is Staph Food Poisoning?

People can get staph food poisoning by eating foods contaminated with Staphylococcus aureus (S. aureus) bacteria. While eating, these bacteria release a toxin onto the food. If you eat too much of that toxin, you can expect a rapid onset of severe nausea and vomiting. It may also cause fever.
Staph contaminates some foods more than others. Protein-heavy foods like eggs, meat, and poultry, as well as sandwiches, salads, and dairy tend to be especially at risk. When these foods are left out at room temperature for too long, staphylococcal contamination risks rise.
How Are Staph Infections Diagnosed?

A doctor may diagnose a minor Staphylococcus skin infection by examining the skin. Lab tests are not usually needed. Serious staph infections of the blood, pneumonia, or endocarditis (inflammation of the inner chambers of the heart) usually require cultures.
In these cases, you may be required to provide a sample of blood, pus, or other tissues. These are then grown in the lab to confirm the presence of the Staphylococcus bacterium.
If staph bacteria are confirmed, another test called a sensitivity test can be run to see which antibiotics will kill the bacteria.
Golden Staph: What It Looks Like
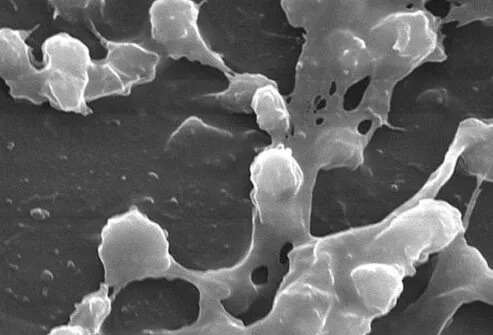
Staphylococcus aureus is fairly small, even by bacterial standards. It's about 40 times smaller than the width of a human hair. It's four times smaller than your red blood cells. It takes a highly magnified microscope to see it at all.
S. aureus appears when growing on agar medium as small, round golden clumps or colonies. When Gram-stained and viewed with a microscope, they appear arranged like clusters of grapes. It gets its name, aureus, from its golden color—an aureus was a gold coin in Ancient Rome. Between and around the round bacterium are thread-like connections of biofilm. Biofilm helps protect the bacterium and increases its chances of causing infections.
How Are Staph Infections Treated?

Treatment for staph infections depends on the location and severity of the infection. Minor skin infections can be treated with topical antibiotic ointments, or oral antibiotics. Abscesses are generally treated with incision and drainage or surgery.
More severe infections in large areas of the skin, other body organs, or the bloodstream are generally treated with intravenous antibiotics. MRSA infections may be resistant to many antibiotics.
Can Staphylococcal Infections Be Prevented?

There is no vaccine currently available to prevent Staphylococcus aureus. . Preventing staph remains the best defense against contracting an infection. Ways to help manage risk factors for contracting staph and MRSA are discussed on the following slides.
Keep It Covered

Cover all skin staph infections with clean, dry bandages. This is especially important if the wounds are producing pus and draining, because the pus may contain MRSA, which can spread to others.
Keep Hands Clean

Proper hygiene is important. Wash hands diligently, avoid close contact with infected individuals, and carefully clean all skin scrapes, cuts, and wounds to reduce the chances of them becoming infected with staph. If you have staph, make sure all people in close contact with you wash their hands frequently, especially if they change your bandages or touch the infected wound.
Don’t Share

Do not share personal items that may have come in contact with the infected wound. Items such as towels, razors, bed linens, or clothing should not be shared. Wash all bedding and clothing in hot water, and dry in a hot dryer to help kill staph bacteria.
Prepare Food Safely

Handle and prepare food safely to help decrease the risk of staphylococcal food poisoning:
- Wash hands thoroughly with soap and water before handling and preparing food.
- If you have wounds, skin infections, or a nose or eye infection, do not prepare or serve food to others.
- Clean and sanitize kitchens and all dining areas.
- Keep hot foods hot (over 140 F) and cold foods cold (40 F or under).
- Refrigerate any food that is to be stored as soon as possible.
Avoiding Toxic Shock Syndrome

Menstruating women may develop toxic shock syndrome. This is a rare, life-threatening illness caused by toxins secreted by staph bacteria and associated with tampon use. The danger is greater when tampons are not changed frequently. The risk can be reduced by:
- Changing tampons every 4 to 8 hours
- Using low-absorbency tampons
- Alternating tampon use with sanitary pads
Retained IUD’s, recent surgery, skin burns and cuts also increase the risk of toxic shock syndrome.
Tell Your Doctor

It may be critically important that you alert your medical staff if you have an infection of staph (especially if it is methicillin-resistant). Tell your doctor or any health care provider you visit so they can take proper protective precautions.
Prognosis

When mild and promptly treated with antibiotics, the prognosis for recovery from a staph infection is excellent. However, a MRSA infection can have an entirely different outlook. MRSA infections, when mild and found in otherwise healthy individuals have a relatively good prognosis. MRSA infections in chronically or severely ill people, the elderly, newborns, or other people with compromised immune systems may be life-threatening or fatal.
Staphylococcal Infections: Essential Facts

- Staphylococcus are bacteria that can cause many types of infections.
- Staphylococcus can cause diseases such as abscesses, impetigo, food poisoning, cellulitis, mastitis, scalded skin syndrome, and toxic shock syndrome.
- MRSA, or methicillin-resistant Staphylococcus aureus, is a type of staph infection resistant to many different antibiotics.
- Staph infections are treated with topical, oral, or intravenous antibiotics, depending upon the type and severity of the infection.
What Is a Staph Infection? Symptoms, Pictures
This tool does not provide medical advice. See additional information: 
© 1996-2024 WebMD, LLC. All rights reserved.
