What Is Pelvic Pain?

Do you know where your pelvis is? Your pelvis is below your belly button in the anterior lower abdomen, and includes your sex organs. Pelvic pain may develop from many diseases and conditions. For example, pelvic pain may come from normal menstruation, appendicitis, bladder problems,; and may be associated with both benign and emergency medical conditions. For most people, pelvic pain should be investigated by a medical professional. A doctor will take the person's medical history, perform an exam, and may order tests to diagnose the cause of pelvic pain. The following slides will present some of the causes of pelvic pain.
Appendicitis
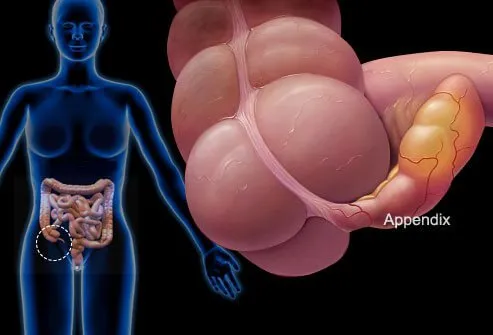
What is appendicitis? Inflammation or infection of the appendix is called appendicitis. Appendicitis often produces lower right-sided pelvic or abdominal pain that may occur along with nausea, vomiting, and fever. An infected appendix usually needs to be removed by a surgeon because it may perforate (burst) and infect the peritoneum and cause life-threatening peritonitis. Removal of the appendix (appendectomy) may be done via several small incisions in the abdomen (laparoscopy) or via one larger incision.
Irritable Bowel Syndrome (IBS)

Symptoms of painful cramps in your pelvic and lower abdominal area, bloating, constipation, diarrhea, and other symptoms that may occur off and on over time are often caused by irritable bowel syndrome (IBS). IBS is a chronic functional disease with recurrent symptoms. It affects approximately 7% to 21% of people. Changes in diet, stress management, and medications are used to treat the symptoms of IBS. More frequent or less frequent bowel movements are both associated with IBS. See a gastroenterologist if you believe you are suffering from IBS. If colon blockage happens (unable to pass gas, severe bloating, abdominal and/or pelvic pain, no appetite), a surgical medical emergency occurs.
A condition known as IBS-C is a subset of irritable bowel syndrome that involves abdominal symptoms along with constipation. This results in less frequent stools, hard stools, or having stools that are hard to pass. People who have this type of IBS may feel as though they have incomplete bowel movements. Some people may feel as though they have a blockage. Changing position or pressing on the abdomen may help them complete their bowel movement. This feeling as though there is a blockage is different than having an actual blockage, which is a medical emergency.
Some conditions involve "pseudo-obstruction" where a person feels signs and symptoms similar to that of an intestinal obstruction. However, there is no actual physical blockage in this condition. Infections, pelvic or abdominal surgery, and conditions that affect muscles and nerves like Parkinson’s disease may cause pseudo-obstruction. Opioid pain medications and tricyclic antidepressants may also produce these symptoms.
Intestinal Obstruction

Intestinal obstruction occurs when part of your intestine is blocked. It may result in death of a part of your bowel or even death of the person. True, physical bowel obstruction is a medical emergency. The condition causes constipation, vomiting, abdominal pain, abdominal swelling, loss of appetite, and an inability to have a bowel movement or pass gas. Potential causes of intestinal obstruction include intestinal adhesions that result after abdominal surgery, colon cancer, diverticulitis, hernias, impacted feces, twisting of the colon (volvulus), and inflammatory bowel diseases such as Crohn’s. A doctor can diagnose a bowel obstruction by performing a physical exam and ordering imaging tests such as X-rays, CT scan, and an ultrasound.
Treatment depends on the underlying cause of intestinal obstruction. A person suffering from bowel obstruction may receive IV fluids for hydration and have a nasogastric tube placed in their stomach to removed fluids and air. A catheter may be placed in your urethra to drain urine. Treatment involves removal of the obstruction and any tissue damaged by the process. Sometimes a stent is placed to force open a part of your bowel.
Painful Ovulation (Mittelschmerz)
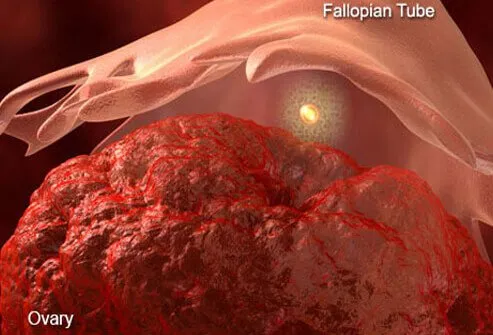
Short-term (hours) pelvic pain that occurs during ovulation (release of the egg from the ovary) is termed mittelschmerz, a German word meaning "middle pain." This pain occurs just prior to, and during ovulation as the membrane that covers the ovary stretches to release the egg. The blood and fluid that are released during ovulation also may cause discomfort or pain. The pain varies from woman to woman and may last minutes to hours. The pain eventually resolves without medical treatment and usually does not require emergency medical intervention. Mittelschmerz is a common cause of gynecologic pelvic pain in women.
Premenstrual Syndrome (PMS)
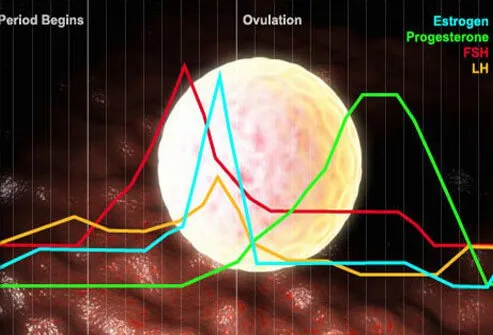
In contrast to painful ovulation described previously, premenstrual syndrome (PMS) usually involves longer term (days before menstruation occurs) pelvic pain and discomfort outside the pelvic area such as low back pain, headaches, tender breasts, and other symptoms. Medications, along with lifestyle changes (diet, exercise, stress management) may often reduce PMS symptoms. This slide shows a chart that illustrates the various hormones that increase and decrease during a woman's normal monthly menstrual cycle. Many women rely on over-the-counter anti-inflammatory medication to relieve pain associated with PMS.
Menstrual Cramps
In contrast to painful ovulation described previously, premenstrual syndrome (PMS) usually involves longer term (days before menstruation occurs) pelvic pain and discomfort outside the pelvic area such as low back pain, headaches, tender breasts, and other symptoms. Medications, along with lifestyle changes (diet, exercise, stress management) may often reduce PMS symptoms. This slide shows a chart that illustrates the various hormones that increase and decrease during a woman's normal monthly menstrual cycle. Many women rely on over-the-counter anti-inflammatory medication to relieve pain associated with PMS.
Ectopic Pregnancy
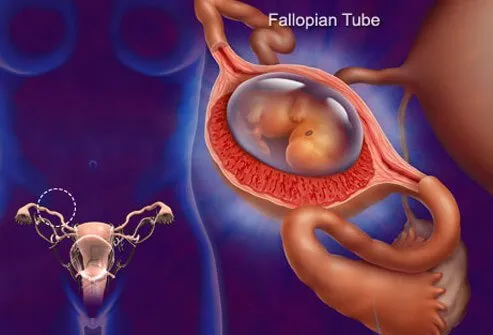
An ectopic pregnancy is growth of an embryo outside of your uterus; it can cause sharp pelvic pain, usually on one side of your body, and may be accompanied by vaginal bleeding, nausea, and dizziness. Ectopic pregnancy, if detected early, may be medically treated, but if heavy bleeding or a Fallopian tube ruptures, it is a medical emergency that requires surgery.
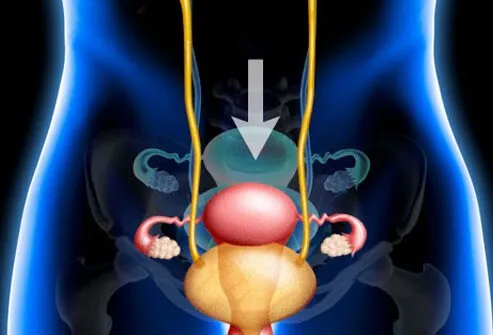
Pelvic Inflammatory Disease (PID)
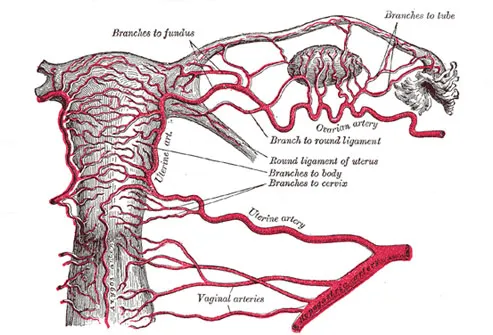
Pelvic inflammatory disease (PID) is an inflammatory and infectious disease, and may be a complication of a sexually transmitted disease (STD) such as gonorrhea. PID can cause damage to your Fallopian tubes, ovaries, and the uterus. Pelvic pain that radiates to your abdomen, an abnormal vaginal discharge, and pain during intercourse or urination are common symptoms. Although antibiotics may cure PID, some women may require surgery. If PID is untreated, it can cause infertility, ectopic pregnancy, and chronic pelvic pain.
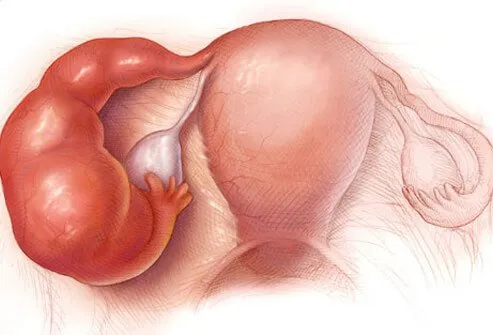
Ovarian Cysts

Ovarian cysts are fluid-filled areas within your ovary formed by fluid that accumulates when a follicle fails to release an egg, or when a follicle recloses after egg release. There are several types of ovarian cysts. Common symptoms include sharp pelvic pain, irregular menstruation, pelvic pressure, or pain after sexual activity and intercourse. Pelvic pain and painful urination may occur especially with large cysts; although most cysts resolve on their own, some may require treatment with prescription medications or surgery to remove the cyst(s).
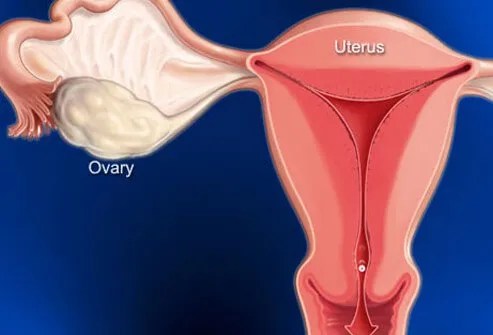
Uterine Fibroids
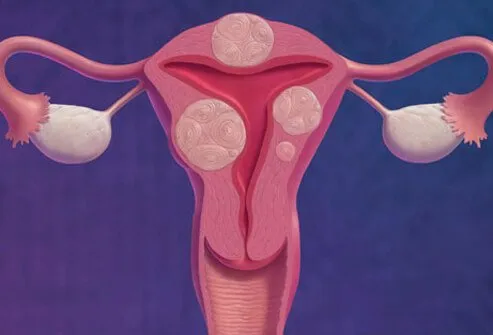
Fibroids are tumors that grow in your uterine wall that are almost never cancerous (benign tumors or growths). Some uterine fibroids cause pelvic pain (mild, moderate, or severe), pain during intercourse, pelvic pressure pain, and may interfere with a woman's ability conceive. Fibroids may cause chronic pain. Uterine fibroids are most common in women in their 30s and 40s. Women that have symptoms should consult their OB/GYN doctor. Treatment may include medication for symptoms or surgical removal.
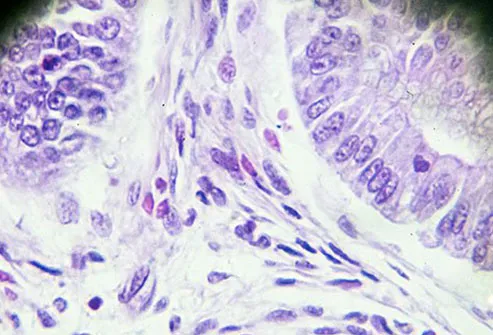
Endometriosis

Endometriosis is growth of the endometrium (uterine tissue) in areas outside the uterus. This tissue may attach to many other organs such as the bladder or intestines or even reproductive organs like the ovaries. This tissue breaks down monthly just like normal endometrial tissue, but the tissue remnant and some blood is retained in the pelvis or abdomen and may cause periodic pelvic and abdominal pain. Treatment is with medication to reduce symptoms; sometimes surgery is required. Endometriosis may also decrease a woman's ability to conceive.
Urinary Tract Infection

A urinary tract infection (UTI) may cause pelvic pain, but usually has associated painful urination (dysuria), frequent urge to urinate, and lower pelvic pressure. UTIs that involve the kidney may have flank pain in addition to fever and nausea. Almost all UTIs can be effectively treated with antibiotics, but delays in treatment can result in kidney damage.
Kidney Stones
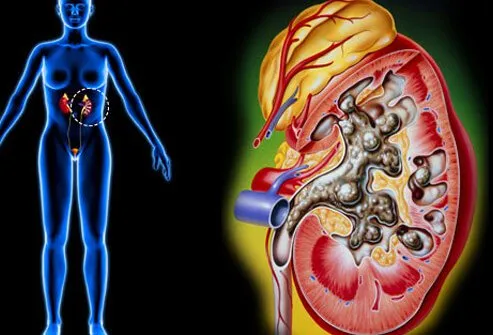
Kidney stones are composed of crystals that usually form in your kidneys or ureters (the tubes that carry urine from the kidneys to the bladder); most kidney stones are very small, but some can be as big as a golf ball. Most small stones cause intense flank and pelvic pain as they irritate the ureters as they pass through them. The urine may contain blood caused by the kidney stone irritating the tissue in the kidney or ureter. Although most stones smaller than 6mm pass spontaneously, they do so with a great deal of pain. Some stones, especially if they are causing an obstruction, may require a urologist to evaluate the patient because the stones may need to be broken up or removed surgically.
Interstitial Cystitis (IC)
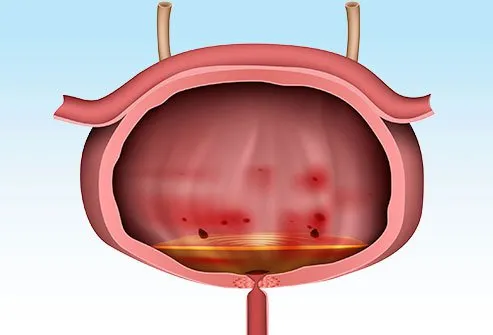
Chronic mid-pelvic recurrent pelvic pain is a sign of interstitial cystitis (IC). Pressure and pain in the pelvic area, the urge to urinate, painful urination, and pain during intercourse also may occur. Although the cause of IC is unknown, there are medications to reduce the symptoms. Like uterine fibroids described previously, IC occurs mainly in women aged 30 to 40, and the cause is unknown.
Sexually Transmitted Diseases (STDs or STIs or sexually transmitted infections)
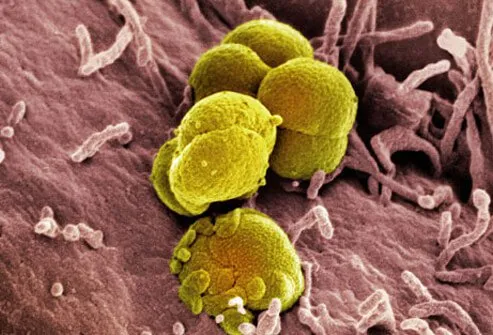
Although sexually transmitted diseases (STDs or STIs) do not always cause pelvic pain, if a person develops pain in the pelvis and has an STD, the pain suggests that complications such as pelvic inflammatory disease, described previously, may be developing. The most common STDs are chlamydia and gonorrhea; less common but important is syphilis. Some strains of bacteria that cause gonorrhea have developed multiple drug resistance and have become very difficult to treat with antibiotics. Viral STDs include genital herpes, genital warts, HPV and HIV that may or may not cause any pain or irritation in the pelvic area.
Pelvic Organ Prolapse
Pelvic prolapse is a condition where a pelvic organ such as the bladder or uterus drops into a lower-than-normal position and in some instances protrude into the vaginal canal. This condition results in pelvic pain that is pressure-like and may include vaginal and back pressure. Usually, there is pain with sex. This condition may occur in older women; treatments range from techniques to strengthen pelvic musculature to surgery.
Pelvic Congestion Syndrome

Pelvic congestion syndrome occurs when pelvic veins become swollen and painful due to low blood flow, just like varicose veins that can develop in the legs. The pelvic pain caused by these veins usually increases with sitting or standing and may be reduced by lying down flat. The treatment may involve medication or embolization (stoppage of blood flow to the affected vein).
Scar Tissue (Abdominal Adhesions)

Scar tissue (also termed abdominal adhesions) forms after abdominal surgery and may make tight connections between organs and other body tissues in your abdomen. Scar tissue may form after any type of abdominal surgery (for example, hysterectomy, C-section, appendectomy). It can cause pelvic and abdominal pain and even compromise blood flow. Some people require surgery to remove these adhesions.
Vulvodynia (Vaginal Pain)

Vulvodynia (vaginal pain) is chronic vulvar pain that includes throbbing, aching, or burning pain in the area around the vulva and vaginal opening. Women also may experience vaginal itching. The pain may be constant or intermittent and is often worsened during sex or when pressure is placed on the vaginal area (bicycle riding, for example). The diagnosis is made by excluding other pelvic pain causes because the cause of vulvodynia is unknown. Treatment is symptom reduction; methods range from home remedies, prescription medication, biofeedback, exercises, and nerve blocks. Some women may be helped by physical therapy that focuses on relaxing pelvic floor muscles.
Pain During Sex

Pelvic pain during sex (dyspareunia) has been discussed as a symptom in most of the conditions described previously. Pain may occur superficially on the surface of the genitals, deeper near the cervix, or anywhere in between. Other causes of painful intercourse not discussed previously include vaginal dryness or atrophy that occurs during menopause or changes in sexual behavior. Diagnosis and treatment of the causative condition usually will reduce or stop pelvic pain that occurs during sex (for example, vaginal estrogen creams or rings to increase vaginal lubrication during menopause). However, some people who have no medical condition diagnosed as the cause of painful intercourse may benefit from consultation with a qualified sex therapist.
Chronic Pelvic Pain

Chronic pelvic pain is often defined as pelvic pain that occurs below your belly button for six or more months. It usually interferes with sleep, it may increase or decrease daily or change due to some specific stimulus or position, and it may interfere with sexual relations. Seeking medical help to obtain a diagnosis and appropriate treatments are the key to diagnosing the cause and resolving chronic pelvic pain.
Adenomyosis
Like endometriosis, adenomyosis is a condition characterized by inappropriate growth of your endometrium, the lining of the uterus. Adenomyosis involves the growth of the endometrium into the outer walls of the uterus. This layer is muscular. Some women do not experience any signs or symptoms of the condition;, however, others may suffer from painful menstruation, pelvic pain during intercourse, and heavy periods. Some women develop a growth inside the uterus called an adenomyoma. The cause of adenomyosis is unknown.
Pudendal Neuralgia
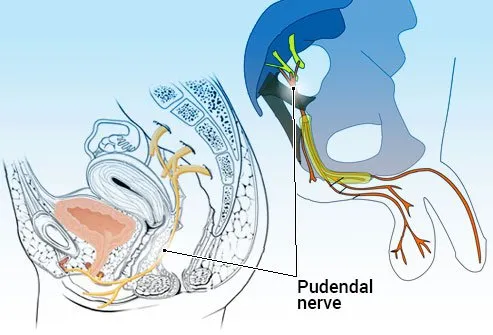
Your pudendal nerve is the nerve of your perineum, the area between the anus and vulva in women or the scrotum in men. Pudendal neuralgia is a pain syndrome that occurs when the pudendal nerve is irritated, damaged, or compressed. This may result in symptoms like pelvic pain and burning and tingling in the genitals and buttocks region. Pain during intercourse, frequent urination, and urinary urgency may also occur. Sitting aggravates symptoms while lying down or standing up relieves them. The condition may occur in men or women, but approximately two-thirds of people who get pudendal neuralgia are women. Underlying causes of the condition include childbirth, trauma, tumors, and infections. Doctors may prescribe physical therapy to treat the condition.
Levator Ani Syndrome
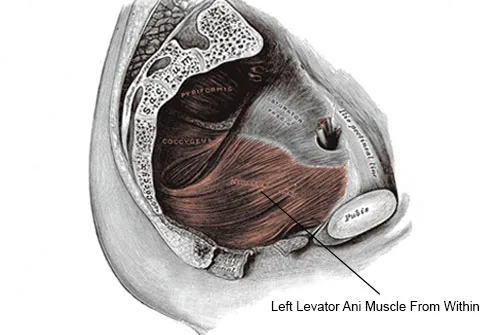
The levator ani is a muscle that lies on both sides of the pelvis. Levator ani syndrome is a chronic pelvic pain condition. People who suffer from the condition get episodic pain in the anus and rectum. It affects both men and women who are usually between the ages of 30 and 60 years old. The exact cause of levator ani syndrome is unknown, although chronic tension in muscles of the pelvis is believed to play a role. Your doctor may prescribe physical therapy, biofeedback, or Botox injections to treat the condition.
Osteitis Pubis

Osteitis pubis is a condition that causes chronic pelvic pain due to inflammation of joints in your pelvis and surrounding muscles. Athletes may experience the condition as well as those who undergo invasive procedures involving the pelvis. A doctor may prescribe rest, physical therapy, and alternating application of ice and heat to relieve symptoms. Osteitis pubis is a rare type of pelvic pain syndrome.
Ovarian Torsion
Many causes of pelvic pain result in chronic pain, however there are some conditions that result in acute pelvic pain. Ovarian torsion (OT) is one such example in which an ovary twists or flips on its attachment to other structures, causing decreased blood flow. It is a medical emergency that may result in loss of the ovary. Ovarian torsion may occur in females of any age from infants to the elderly. The condition may be diagnosed by ultrasound (usually transvaginal ultrasound) and is treated with surgery.
Pelvic Pain: What's Causing Your Pelvic Pain?
This tool does not provide medical advice. See additional information: 
© 1996-2024 WebMD, LLC. All rights reserved.
