What Is an Appendix?

Your appendix is a small, pouch-like sac of tissue at the beginning of your large intestine. It can be found on the right side of your body in an area in your lower-right abdomen called the "cecum." The full name of your appendix is "vermiform appendix," which means "worm-like appendage."
What Does Your Appendix Do?
For many years, the appendix was considered useless. Doctors found that patients were apparently healthy after removing their appendix. That image has changed more recently. Researchers have found that your appendix plays an important role in boosting your immune system.
Your appendix harbors gut bacteria. This helps your digestive system recover after an infection. For example, bacteria from your appendix help repopulate your colon after a bout of diarrhea, helping you recover faster. It also seems to protect against Chron's disease, a common chronic bowel disease. Patients with an intact appendix are four times less likely to develop UC.
What Is Appendicitis?
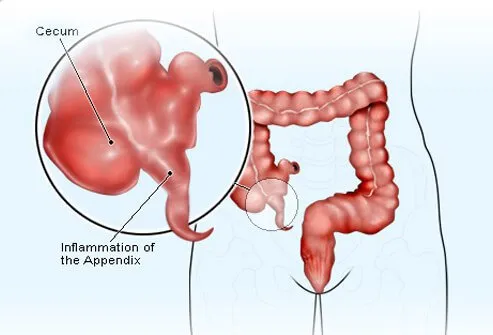
The suffix "-itis" means "inflammation" in English, so appendicitis is inflammation of your appendix. Appendicitis can occur when mucus, stool, a growth, or a combination of these blocks the opening of your appendix that leads to the cecum. It may also be caused by abdominal trauma or inflammatory bowel disease. In each case, bacteria proliferate in the trapped space and infect the lining of your appendix.
What Causes a Ruptured Appendix?
If the inflammation and blockage are severe enough, the tissue of your appendix can die and even rupture or burst, leading to a medical emergency. The risk of a ruptured appendix becomes greater the longer treatment is delayed for appendicitis.
Who Gets Appendicitis?

Anyone can get appendicitis. But it occurs most often in people between the ages of 10 and 30. Men have a higher risk than women. About 7% of people in the U.S. experience appendicitis during their lifetime. Very young children and elderly people are at higher risk of complications. Early recognition and prompt treatment of the condition are necessary, especially for more vulnerable people.
Appendicitis: What Is Perforation?

Delaying the diagnosis and treatment of appendicitis increases the risk of complications. One potential complication -- perforation -- can lead to an accumulation of pus (abscess) around your appendix or an infection that spreads throughout the abdominal lining and that of the pelvis (peritonitis). Surgery should occur as soon as possible after the diagnosis of appendicitis. Longer delays between diagnosis and treatment (surgery) increase the risk of perforation. For example, the risk of perforation 36 hours after appendicitis symptoms first appear is 15% or more.
Intestinal Blockage
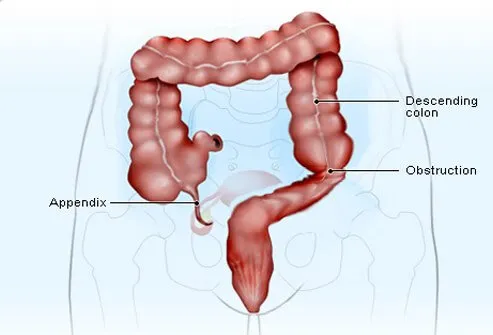
Sometimes the inflammation associated with appendicitis interferes with the action of the intestinal muscle and prevents bowel contents from moving. Nausea, vomiting, and abdominal distention can occur when liquid and gas build up in the part of the intestine above the blockage. In these cases, a nasogastric tube may be necessary to drain the contents that cannot pass. This is a tube inserted into your nose that advanced down your esophagus into your stomach and intestines.
Appendicitis Symptoms

One of the earliest appendicitis symptoms is abdominal pain that is hard to pinpoint. People with appendicitis typically experience pain in the central part of their abdomen that eventually moves over to the right lower quadrant (McBurney's point). Loss of appetite is another early symptom of appendicitis. Nausea and vomiting may occur early in the course of the illness or even later as the result of an intestinal obstruction.
Some of the symptoms of appendicitis include:
- Pain near the center of your abdomen that eventually moves down your abdomen along your right side
- This pain gets worse in a matter of hours, and it may hurt when you cough, sneeze, or move around, or breathe deeply
- Stomach problems like nausea, vomiting, loss of appetite, constipation, or diarrhea
- Trapped gas
- Low fever
- Stomach swelling
- Feeling the need for a bowel movement to relieve discomfort
Diagnosis

Doctors diagnose appendicitis based on the patient's symptoms and findings during physical examination. A person with appendicitis usually experiences moderate-to-severe pain when the doctor gently pushes down on the lower right abdomen. A potential indication of peritonitis is "rebound tenderness," which is a worsening of pain when the doctor removes his hand after pressing down on a tender area of the abdomen.
What Is an Appendectomy?

Surgical appendix removal is called an appendectomy. There are two main types of appendectomy: open and laparoscopic. Open surgeries use one long slit down your side to remove your appendix.
Appendectomies performed laparoscopically use special surgical tools. These are advanced into your abdomen via several small incisions. This type of surgery is associated with less pain and quicker recovery. Antibiotics are given to a patient with suspected or confirmed appendicitis both before and after surgery. The following is a step-by-step account of a laparoscopic appendectomy.
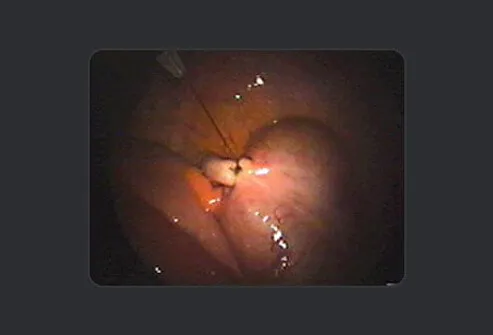
Appendectomy Step by Step: Step 1
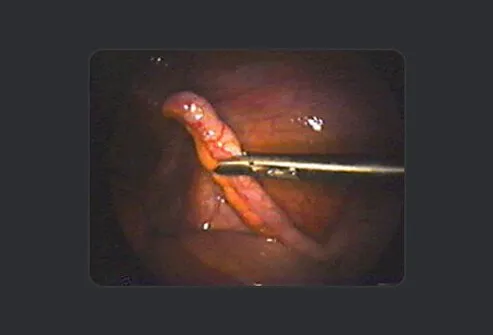
This image shows a normal appendix in a female patient undergoing surgery for an infection in her reproductive system. Since there is no known function of the appendix and to prevent diagnostic confusion in the future, the surgeon removes it to prevent potential appendicitis in the future.
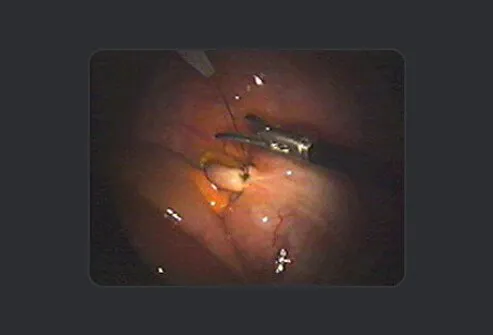
Appendectomy: Step 2

To remove the appendix, the surgeon separates it from the mesentery, which is the tissue that delivers blood to the area. Electric current delivered by bipolar forceps are used to seal (cauterize) the blood vessels and prevent bleeding.
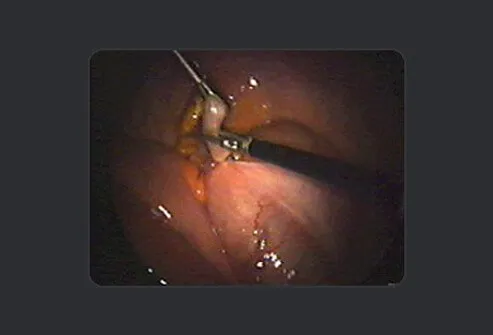
Appendectomy: Step 3

In the next step, the surgeon uses scissors to snip the appendix free from the mesentery. He alternates between electrocautery (to seal blood vessels) and cutting to completely separate the appendix from the surrounding tissues until the only remaining connection is to the colon.
Appendectomy: Step 4
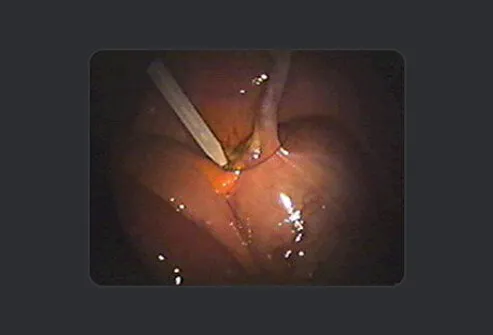
In the next step, the surgeon crushes the base of the appendix with a clamp and then moves the clamp slightly towards the end of the appendix, positioning a pre-tied suture at the base of the appendix to tie it off.
Appendectomy: Step 5
The surgeon tightens and secures the suture using a fisherman's knot, which can be tightened but is incapable of loosening by itself.
Appendectomy: Step 6
The surgeon then uses the scissors to cut the suture above the knot.
Appendectomy: Step 7
The surgeon cuts the appendix with the same scissors above the knot but below the clamp to prevent contamination.
Appendectomy: Step 8
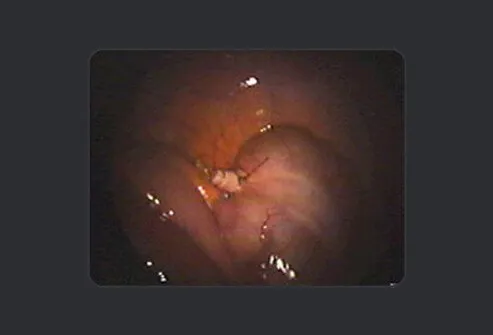
The surgeon and his surgical team complete one final inspection of the area to ensure there is no bleeding.
Potential Consequences of Appendectomy

Infection at the surgical sites is the most common complication associated with an appendectomy. Redness and pain may be present with a mild infection. Moderate infections may have more severe symptoms. Antibiotics are used to treat mild-to-moderate postsurgical infections. If an abscess develops, drainage may be necessary.
The appendix plays an uncertain role in adults and older children. Removal of your appendix is not associated with any major long-term health problems. Some studies report an increased risk of certain diseases after an appendectomy. Crohn's disease, which is an inflammatory intestinal condition, is one such disease.
Appendectomy Recovery

Right after surgery, you will be stitched up and taken to a recovery room. Your medical team will keep watch over your vital signs as you wake up from anesthesia. When you wake up, you will find a sterile bandage around your surgical wounds.
Recovery times differ based on surgery. After laparoscopic surgery, you may be sent home the same day. Patients are given pain medicine, and may need to keep a thin tube through your nose. This tube, which travels to your stomach, clears stomach fluids and any trapped air inside your stomach as you recover. Expect to follow up with your healthcare provider over the next two to three weeks.
Appendicitis: Symptoms, Signs, Causes, Appendectomy in Detail
This tool does not provide medical advice. See additional information: 
© 1996-2024 WebMD, LLC. All rights reserved.
