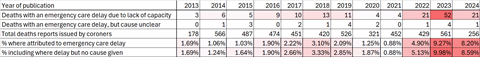
- Share of “prevention of future death” reports where emergency care delays and capacity were cited increased at least three times
- Coincides with huge increases in waits for ambulances and admission to emergency departments
The number of coroner warnings issued last year which were linked to a lack of capacity in emergency care was around four times that seen before covid.
HSJ analysis of “prevention of future deaths” reports – also known as Regulation 28 reports – show a steep rise since 2021 in deaths linked to long delays in ambulance responses, hospital handovers, and emergency department waits.
There were 52 in this category in 2023. The largest number pre-covid was 13 in 2018, although the rate also appeared to be slowly rising in the years running up to 2020.
The reports are issued when they believe a person, company or public body needs to make some kind of change to prevent future deaths. They cover everything from road traffic accidents to buildings regulations.
HSJ analysed more than 5,000 prevention of future death reports dating back to 2013 to better understand the impact of pressures to emergency care services.
It showed nearly 10 per cent of all reports published in 2023, and more than 8.5 per cent of those published so far this year, described deaths involving ambulance or emergency department delays. Back in 2018, this figure was less than 3 per cent.
The steep rise since mid 2021 (see map/chart below) coincides with huge pressures on emergency care, with extremely steep increases in ambulance waiting times, and in very long waits for admission to hospital. Waiting times for accident and emergency assessment also rocketed.
Evidence has linked very long waits in A&E to higher mortality. There was a small improvement in performance overall in winter 2023-24.
The bulk of the PFD reports describe issues with resourcing, but a small number do not give a specific cause for the delays (given in the second row in the table above). Reports that only described failings other than capacity and resourcing issues, such as miscategorised calls, were excluded from the analysis.
Analysing the seasons of the dates of the deaths, HSJ found a sharp increase in reports involving emergency care delays from the summer of 2021 onwards, when 10 deaths triggered PFD reports.
This figure then more than doubled to 24 deaths resulting in PFDs linked to emergency care delays in winter 2021-22. The following winter, 2022-23, saw a further increase, with 27 PFD reports involving emergency care delays.
It takes an average of 1.7 years for a coroner to publish a prevention of future death report after someone has died, so it’s likely many more will be published concerning deaths from the winter of 2022-23 onwards.
Map: Pause the timeline and hover/click points for more information
However, the analysis suggests the seeds of the emergency care crisis were planted long before the 2020 pandemic, with coroners publishing a growing number of reports on the subject from 2015 onwards. A fall in publications in 2020 and 2021 may have been influenced by lower attendances and calls during acute covid peaks, and delays to inquests during the pandemic.
Adrian Boyle, president of the Royal College of Emergency Medicine, said the figures were “upsetting.”
“When a death occurs, relatives and staff want to be assured that they have done everything that could have been reasonably expected. Knowing that there were deficiencies in care is hard for both relatives and clinicians,” he said.
“This problem is fixable with the right policies, which must urgently increase capacity in the whole urgent and emergency care system.”
NHS England said in a statement: “Our deepest sympathies remain with the families affected in these reports and NHS England is continuing to take action to support hospitals to provide safe, high-quality care for patients.”
It said there had been “considerable progress in the recovery of urgent and emergency care services” last year and added: ”It is clear there is still further to go” and pointed to plans for more direct referrals to same day emergency care; ‘step-up’ virtual wards; and “targeted support for patients who regularly attend A&E”.
Updated 28 May at 3.18pm with a comment from NHSE, which had previously not provided a comment.
Source
Prevention of Future Deaths reports
Source Date
2013-2024


























12 Readers' comments