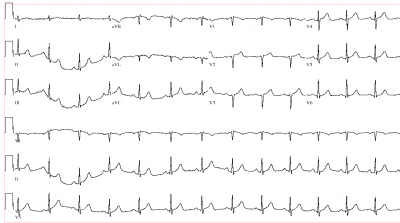
9/30: Update: due to popular demand, I have added the EKG to the end of the post, with some follow-up.
I sent a guy with a normal EKG to the cath lab. Let me tell you my side of the story.
Dude was minding his own business when he started having crushing, substernal chest pain. I see dude by EMS about 45 minutes into his chest pain. He’s had the usual: aspirin, 3 SL NTG’s an IV, a touch of MS (I can abbreviate here, as it’s not a medical record) and is continuing to have pain.
He describes it like you’d expect (elephants have a bad rep in the ED), and looks ill. Frankly, he looks like a guy having an MI. Sweaty, pale, uncomfortable, restless but not that ‘I’ve torn my aorta’ look. The having an MI look.
Every EM doc knows the look. I didn’t ask about risk factors.
On to the proof: the EKG. EMS EKG: normal. ?What? Yeah, maybe there’s some anterior J-point elevation, but not much else. Our EKG: Normal.
Normal EKG’s, patient who clinically looks like he’s having the Big One.
I’d like to tell you I agonized over the decision, but I didn’t. Cath lab called, Interventional Cardiologist says he’ll meet the patient in the cath lab. (Insert excellent nursing and tech care here; time to cath lab 28 minutes, no labs back yet).
Excellent tech comes to me after transporting patient to cath lab. “The cardiologist wanted to know why you sent him a patient with a normal EKG”. ?Are they going to do the cath? I asked. “Yes, but he wasn’t happy”. Supportive team thinks I did the right thing, but, sending a guy with a normal EKG to the cath lab? I don’t blame them for some averted gazes.
Cardiologist comes looking for me an hour later. Doesn’t look happy.
C: Why did you send that patient to the cath lab?
Moi: He was having an MI.
C: He had a totally normal EKG.
Me: Yes.
C: What made you think he was having an MI?
Me: He looked sick.
(An aside: I could have whipped out some BS about some minor historical feature, blathered on about his elevated J points, etc, but I’m stupid and just said what I meant).
C: After I started the cath, another cardiologist looked at the EKG, and agreed it was normal.
Me: (Sinking feeling) And?
C: 100% LAD occlusion, high proximal. I stented it and now he’s good.
Me: So, good?
C: It’s the first patient with a normal EKG I’ve cathed, and he had a 100% LAD occlusion.
Some small talk later, the cardiologist leaves. I have no doubt the cardiologist cannot decide if I’m an idiot or a savant.
I’m neither. I’m an ER Doc. Who got lucky.
Updated:
First troponin was normal; second, several hours later, was nearly 30 (with our high normal being 0.05).



I’m sure you felt better about this “lucky call” than your shooting score.
I had the same symtoms and in the end, the same results. In my case, I like to think that the doctors and nurses at King Bhumibol Adulyadej RTAF hospital knew their stuff and knew it well. Luck has little to do with it sometimes.
Hmmm Good call, I’m just a Gas Passer, but even I remember that its “Not Uncommon” to have a Cold Stone Steve Austin Normal EKG while your Myocardiums Infarctin worse than Dick Cheney at a Green Piece March…
I’d have told him to take his Fa…I mean himself back to his money makin machine and GTFOMER… Cardiologists are big Sissys in my experience…
I mean when someone sends me business I usually buy em a Beer, or a Fresca if they don’t drink…
And I’m an Idiot AND a Savant…
Frank
And was this guy American Trained??? Every real Amurican Doc knows the “Looks Sick as Shit” sign (L-SAS) trumps all others…
Unless its a Shrink or Flea…they think EVERYONE looks sick…but then they’re usually not from around here…
Frank
WOW! I want you in ER taking care of me if the need ever arises! GREAT call!
Just a med student here, but I’ve been taught by both cardiologists and EM docs (and just about every relevant text/article I’ve read) that a NL EKG does not rule out MI. Pertinent positives on presentation are more important than negative tests, right? You could have waited for the EKG to become abNL after a lot more damage, but instead you probably preserved a lot more of his cardiac muscle. Great job!
Experience still counts, fortunately. Knowing/understanding that you’ll be second-guessed is no fun, but it’s the patient’s welfare we signed up to maximize, not our own anxiety level. Call it luck, be humble and describe yourself as an “idiot” or “savant” or whatever floats your boat. Experience still counts and is the only way to recognize L-SAS. (“I may not be able to define L-SAS, but I know it when I see it.”–with apologies to Hugo Black)
Bravo.
And Mr. Davidson, surely you mean “with apologies to Potter Stewart”
Experience trumps an ECG any day.
A colleague and I were discussing several recent cases we’ve seen where pts were having MIs with normal ECGs – but it has been the circumflex artery. Pretty impressive to have 100% LAD occlusion and no ECG changes, not even hyperacute Ts.
Nice call!
You should keep a copy of the EKG and cath report handy for the next time the cardiologists give you a hard time.
I work in a nationally recognized heart hospital and it is not uncommon for the cath lab transport team to be pushing the stretcher out of the ER 10 minutes after arrival, often despite normal EKGs, and our docs are usually dead on (no pun intended) with their gut feelings. Way to stick with your knowledge over gadgets on that one!
Can’t say I’ve ever done that, Grunt… nice work.
I demanded a dood w/o chest pain (felt “SOB” and had trending downward vitals) and ST depression be sent to the cath lab once. “Do I ever make crayzee suggestions like this?! Am I ever wrong when I do?” No, and no…
Doc agreed that something was fishy with the heart MAYBE and the patient was on a balloon pump a little while later…
Way to go. Super job!!
Reminds me of the time I insisted to the surgeon that a patient had appendicitis. He had been in the ED 2 consecutive days. Both times with normal WBC and normal CT. The surgeon VERY reluctantly admitted the guy and finally took him to the OR two days later to take out his perfed appy. Clinical diagnoses still exist for us old farts.
Funny how that whole “Treat your patient, not his test results” theory works sometimes. On the flip side how many people walk into the ER and get the full CBC,BMP, LFT’s, D-dimer, cheast x-ray and full body CT for a case of the 3 am sniffles?…. Good call too bad more MD’s don’t have the balls to follow their instinct instead of practicing defensive medicine.
sounds like you deviated from the chest pain guidelines re: cath lab. may your “quality performance” scores suffer accordingly. :)
To mean this scream Wellen’s waves. I assume you had no prior ECG? I would bet he had deep T wave inversions in his anterior leads that pseudonormalized during his massive MI usually associated with a Left main or high LAD lesion.
Good call too bad more MD’s don’t have the balls to follow their instinct instead of practicing defensive medicine.
If I were you, I wouldn’t judge ’till you’ve been there.
Hey Doc,
Any info on the labs after the cath (Trop, CK, etc)? Curious to see if the lab picked up anything after the fact.
Also curious if an 80 lead EKG could have picked it up.
http://www.primeecg.uk.com/prod_overview.html
Wellens/ Pardi T -waves.
I would like to see that EKG.
Actually, reading the post, it occurred to me that the other thing it could be was Takotsubo syndrome
http://en.wikipedia.org/wiki/File:Takotsubo_ECG.JPEG
http://en.wikipedia.org/wiki/Takotsubo_cardiomyopathy
Of course, that can only be appreciated under flouroscopy.
Good pickup.
For the record, I don’t think that it was luck.
Well, maybe a little, but the reasoning was sound.
Would be good, but there’s still the cath that showed 100% occlusion.
I’ll try to get the EKG and post it here.
This kind of harkens back to that guy with chest pain who expired in the LA hospital waiting room last year. There was a discussion then about whether the triage nurse should have done an EKG on him and whether that was adequate to R/O an MI. Gruntdoc’s case shows that an EKG is no substitute for clinical judgment.
This is not a slam on triage nurses by the way, the great majority of them are great.
Well, I can quite clearly see the lesion with my retrospectacles on.
j/k!
There might be a little bit of *very* early ST elevation in v1-v3. What I see, though, is a biphasic P wave or twp anteriorly. I saw that (in the setting of knowing its an LAD occlusion) and I had a flashback to my days in the Cardiac ICU with Dr. M______, as the fellow telling me the following: “If you see biphasic P-waves in V1 and V2, that’s it; the guy is having an MI.”
It stuck with me because… well, Hell, I don’t know why it stuck with me, but I managed to recall it.
Still, I doubt I would have called the cath lab. I might have done a repeat in ten minutes, but that would have been ten minutes more of significant myocardial tissue death.
It wasn’t luck; you made a great call.
Just further proof that intuition and experience will trump test results every day. When people are really sick, they look crappy.
You are very talented. The patient is the one who got lucky. It’s a good thing he saw you before he saw the cardiologist.
Was a right sided EKG performed?
You listened to your inner voice, wherever it came from.
I don’t believe anyone understands the feeling you had and said, I must do this.
It happens to me all the time, and I learned to listen to it.
The ability to do that is what makes Doctor’s special.
Great Job, you save another life.
Good call! I can’t help but wonder if some genius at the insurance company will try and deny the procedure saying it was “un-warranted”! I remember reading and hearing that 12-leads aren’t always 100% in ruling MI out OR in, so if they look sick I treat THEM (M.O.N.A) and literally glance at the 12 lead (and the computer interpretation AFTER I formulate what I think it is). I always go with my gut, too- especially if they look “C.T.D.-y” (circling the drain-y)…again, GOOD CALL, I don’t think there was much luck, I think it was your training and experience culminating with circumstance and timing…and, thankfully, that guy benefitted!
No luck about it doc, it was experience and that funny feeling in your gut. Oh, that and the patient presented with crushing chest pain and had “the look”.
Good Call. You treat the patient, not the lab value and not the imaging.
One of the most underrated skills in medicine is the ability to recognize when a patient’s about to take a severe turn for the worse, all too often labs/imaging/etc. are lagging indicators..
A GOOD ER DOC IS WORTH HIS/HER WEIGHT IN GOLD.
AT 50 YRS OLD PRESENTED TO ER ON FRIDAY WITH THE ELEPHANT ON MY CHEST(EVERYONE DESCRIBES IT LIKE THAT). NORMAL EKG BUT NITRO RELEIVED PAIN. WAITED IN ER FOR 7 HOURS WHILE LABS WERE DRAWN AND FOR ROOM IN TELEMETRY. WHEN CARDIAC ENZYMES CAME BACK HIGH DR CAME BACK WITH CONFIRMATION OF MI(LIKE I NEEDED HIM TO TELL ME).
GOT CATH ON MONDAY HAD 90% OCCLUSION OF LDCA. GOT STENT BUT GOING BACK 7 YEARS LATER.
“if it looks like a duck, quacks like a duck………”
STRONG goddamn work…
Great story. I’ll be using this as a teaching scenario in the morning.
The ECG isn’t normal (poor R-progression, old anteroseptal MI, Q in aVL). There is some J-point elevation in V1 and V2 as well. If the LAD was 100% occluded it raises the possibility of a prior anterior MI with a chronic total occlusion. The Troponin elevation could be PCI related in that case.
Great case…. Reminds me of a minor leaguer i saw a few years ago as a second opinion prior to a procedure to stabilize his ankle. He denied any precipitating trauma, or any prior history of ankle sprains. Something didn’t make sense. A very focused physical showed what I thought to be slight, asymmetric peroneal weakness. I decided to order an MRI of the spine… the patient, his dad and coach thought I was nuts, until we found a schwanoma wrapped around one little rootlet. Sometimes it just pays to listen to that little voice.
My lucky day: 52yo WM comes in about 11PM, onset that evening of low cervical neck pain. Agitated, keeps walking up and down the hall, rubbing his neck. Hx neg, Exam neg. No sweaty, clammy, etc… Nagging thought: people with disks/strain don’t move around a lot, do they?
OK, so you know the bottom line. But everybody looked at me funny when I ordered the EKG. Bingo.
So, I had seen patients with mid-back pain and MI, and patients with anterior neck pain and MI. But not focal cervical pain.
Yeah, yeah, not unheard of…but, index of suspicion needed.
Cardiologist came around in the morning: “what made you suspicious?”
I think I cathed this guy last night!
The EKG was Abnormal but good call!
The guy was having a “stuttering” MI, if you will. At least that’s the possibility. It’s not a “normal” ecg–but not an obvious STEMI either.
I had this happen the other night. Initial ekg negative but then on a repeat the guy’s got just about 1mm elevation in 2, 3, AVF with some chest pain. The next minute his pain is gone and the ekg is normal. Cath the next AM–after some more chest pain shows clot in the circ. Not a true “stemi” for more than the 2 minutes it took to get ONE ekg in between 3 normal ekgs.
It’s possible your guy was alternating between perfused and not-perfused. ST’s can come and go. Perhaps in the lab his STs were up.
Of course, the alternative is he simply had no major electrical abnormalities. ;-)
Good case.
Dear Pedants:
Yes, I know this EKG isn’t “Normal”; what it’s not is normal for a guy with a 100% LAD lesion who’s visibly having a heart attack in front of you.
Jeez.
Give me enough time and a cath report of 100% LAD, I could probably find a MI in a Laerdal simulator. I’m more surprised the cardiologist chose to stent a proximal LAD instead of going for a CABG.
That EKG is just as normal as 99% of the folks who get discharged from the ED every day. Based on the information available to you AT THE TIME it was a heck of a good call.
Sent a guy to the lab with a 100% circ to the lab with a normal EKG just two days ago.
Go figure.
And sorry to be pedantic. Or something. ;-)
And apparently I like repeating myself myself.
Keep up the good blogging!